How is the removal of a herniated disc in the cervical spine
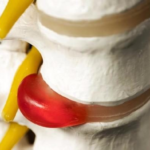
A hernia of the cervical spine is not diagnosed as often as in the lower back or chest region, but its consequences are most dangerous. A protrusion of the intervertebral disc of the neck without treatment leads to a violation of cerebral circulation, an increased risk of stroke, memory and overall quality of life deteriorate.
Removal of a hernia in the cervical region is not always required. Treatment is often carried out by conservative methods, for which medications, physiotherapy and exercise therapy are used. But when the hernia is large and begins to pose a threat to health and life, the option of surgical intervention with partial or complete removal of the damaged disc is considered.
Removal of a hernia of the cervical spine depends on the degree of danger; at the initial stage, surgery is not required, but at the stage of sequestration, radical treatment is indispensable.
Treatment of a hernia of the cervical spine
The operation to remove a hernia of the cervical spine refers to complex interventions at any stage of the disease. In surgery, planned and emergency treatment methods are distinguished, but each has a number of limitations and requires special training.
There are the following stages of the formation of a herniated disc in the cervical region:
- Prolapse - detachment of the fibrous ring without deformation.
- Protrusion - partial protrusion of the fibrous ring.
- Extrusion - rupture of the annulus fibrosus with swelling of the pulp.
- Dysfragmental hernia - the nucleus pulposus comes out only at the moment of movement, returns to its place at rest.
- Sequestered hernia - rupture of the fibrous ring and separation of the pulp with its free movement along the spinal canal.
Surgery for a hernia of the cervical spine will be mandatory in case of a sequestered hernia. This is the only absolute indication, while other severe conditions can still be supported by conservative methods.
Indications for surgery
In what cases can the removal of an intervertebral hernia be prescribed:
- pain syndrome for several months;
- sequestered hernia;
- infringement of the nerve roots;
- severe neurological symptoms;
- severe deformation of the vertebra and disc;
- cauda equina syndrome with dysfunction of the pelvic organs;
- infringement of the spinal cord;
- irreversible damage to the tissues surrounding the disk.
Conservative treatment will not give a result when the patient does not comply with the requirements of the neuropathologist and traumatologist. The reason for radical removal may be concomitant endocrine pathologies, a congenital disease of the bone and connective tissue, when degenerative changes cannot be treated with drugs and physical methods.
The choice of surgical technique will depend on the type of disease, location, size, and stage. There are 2 groups of hernias in the cervical region: anterolateral and posterolateral.
Posterolateral formations are lateral, paramedian and median. Ventral or anterolateral hernias are detected very rarely, which is associated with a slight load on the anterior part of the annulus and a strong longitudinal ligament. More often, a protrusion of the disc is diagnosed in the C5-C6 region, less often between the C4-C5 and C7-T1 vertebrae.
Contraindications
Spine surgeries have common contraindications:
- decompensated heart disease;
- malignant neoplasms;
- period of pregnancy;
- infectious diseases;
- blood clotting disorder.
A herniated cervical spine will be treated conservatively if the risk of surgery outweighs the potential benefit. When there are relative restrictions on the operation, the patient has the right to make his own decision after listening to the opinion of the doctor. Surgery will always be recommended by surgeons when there is a risk of paralysis and complete disability. A contraindication will be a recent stroke, severe neurological disorders, intolerance to anesthesia, encephalopathy and other dangerous conditions.
Preparation
Before the operation, you will need to undergo a series of studies, look around with several specialized doctors in order to exclude possible contraindications and prepare the body for surgical intervention.
Full preparation includes the following activities:
- Examination of the cardiovascular system and respiratory organs . Many postoperative complications are associated with the respiratory and cardiovascular systems, therefore, before treatment, the patient undergoes a second examination, echocardiography, chest x-ray, spirography, electrocardiography are prescribed.
- Dental treatment and examination by an otolaryngologist . It is important to eliminate all foci of infection in the body, including carious cavities, stomatitis, tonsillitis, it may be necessary to remove the tonsils in case of their chronic inflammation.
- Assessment of the state of the liver and gastrointestinal tract . Fibrogastroduodenoscopy, ultrasound of the abdominal cavity is performed to exclude peptic ulcer and liver pathologies.
- Blood test, hematological examination . To detect metabolic disorders and diagnose inflammatory foci in the body.
A weakened body before surgery requires special preparation. The patient is prescribed vitamin complexes, hormonal agents, immunomodulators. Alcoholic beverages, smoking, drug use must be excluded.
Before the operation itself, the doctor may prescribe a second x-ray and MRI of the cervical spine.
discectomy
A radical method of treatment is discectomy, the hernial protrusion is removed and then the entire nucleus pulposus is removed. The operation is performed through a skin incision over the defect itself. To create access to the protrusion, the disc is removed, the nerve root is retracted, and the hernia is excised. Excision of the entire pulp reduces the risk of recurrence.
The patient after discectomy is in the hospital for 2 weeks. The rehabilitation period is 2 months, during which physical activity is prohibited. For 2 months after the operation, you can not sit, it is recommended to wear a rigid postoperative bandage and follow a diet. Physical activity is allowed from 4 months after the operation.
A discectomy can be performed with a laminectomy, the removal of the nerve root. This approach is necessary only in the case of spinal stenosis.
Microdiscectomy
Microsurgical discectomy is performed for hernia with compression of the nerve root, this operation is the gold standard of treatment. A microdiscectomy is performed under anesthesia, access is created over the damaged disc. The operation is different in that the removal of the disc is not required, the surgeon gains access to the formation by biting out the ligament of the intervertebral foramen.
A microscope is used during the operation. To reduce the risk of recurrence, additional laser irradiation may be performed after hernia removal.
This technique does not violate the motor function of the operated area, and prevents relapse. The patient is discharged on the 5th day. You can sit after the operation, but not for long, a light load is acceptable, but you can lift no more than 2 kg, while you can not make sharp turns, bends, jumps.
You can return to physical work in a month, but lifting more than 5 kg is permissible only for the 3rd postoperative month. It is recommended to work in the first weeks in a supporting semi-rigid corset.
laser removal
Laser treatment involves the evaporation of a hernia by introducing a light guide through the skin. The dosed energy turns the liquid into vapor, which is then expelled through the needle. The operation allows you to reduce the pressure inside the disc by reducing the size of the protrusion. This anesthetizes, reduces pressure on the nerve roots and reduces the number of pain receptors. This method does not apply to surgical methods of treatment, the diseased disc continues to disturb, and the procedure will need to be repeated soon.
What is the difference between laser treatment of disc herniation:
- after the laser there is no scarring, minimal tissue injury;
- the possibility of repeated treatment and irradiation of several segments at once;
- no damage to nerve structures;
- the doctor controls the course of the needle according to the patient's feelings;
- local anesthesia is applied.
Vaporization
Soldering or vaporization of the disc is the type of laser treatment that is most often used. During the procedure, the laser beam acts on the diseased disc, moisture evaporates, which reduces the hernia, and with it the symptoms.
The method is indicated for patients with protrusion of the intervertebral disc at the age of 20-55 years at an early stage of the disease, when there are no indications for radical removal. Vaporization is suitable for protrusion and at the stage of destruction of the fibrous ring, when the pulp remains intact or slightly extends beyond the core.
With degenerative changes and in old age, vaporization is not always suitable, but can be considered as an additional method of minimally invasive treatment.
The procedure has both a therapeutic and prophylactic effect, preventing further disc displacement and the appearance of sequesters.
Reconstruction
Laser reconstruction involves heating the damaged disc, which starts the recovery process. After the procedure, there is an active growth of cartilage tissue, which gradually replaces the cracks in the disc. The process helps to get rid of chronic pain syndrome.
Reconstruction is performed using a thin needle that is inserted into the area of the diseased disc. The procedure is carried out only in stationary conditions, the patient stays in the hospital for 2-3 days. The technique can be considered as an independent procedure and a method of postoperative recovery.
Endoscopic removal
The operation with the use of an endoscope is performed under local anesthesia. The instrument is inserted through a puncture, the surgeon watches what is happening on the screen, removing the hernia and nucleus pulposus. The tissue incision is made approximately 5 mm, and the endoscope itself has a diameter of 4 mm. This procedure is considered the least traumatic of all presented, it reduces the risk of a doctor's mistake, as it is carried out under visual control.
The rehabilitation period after endoscopic surgery is short - up to 3 days in the hospital and a month of home recovery, after which you can return to your usual lifestyle and professional activities.
Postoperative rehabilitation
The rehabilitation program is developed for each patient individually, and includes activities to strengthen the natural muscular corset of the spine. After the operation, 3 recovery periods are distinguished: early, late and remote. The latter has no conditional boundaries and continues throughout life.
The first 14 days after discectomy, the patient observes bed rest, excludes any load and stressful situations. Measures are being taken to prevent early complications, relieve pain and swelling of tissues. The doctor prescribes drugs, daily dressing of the wound and wearing a postoperative bandage.
Features of rehabilitation after removal of a hernia in the cervical spine:
- Early period - 2-8 weeks . The body's adaptation time to light loads, anesthesia is carried out, spinal blocks are prescribed, light exercises for relaxation and muscle stretching are gradually included in the regimen.
- Late period - the first year after the operation . The attending physician monitors the condition, prescribes physiotherapeutic procedures, gymnastics, and regularly examines the patient. The main goal of rehabilitation will be the complete restoration of the function of the operated spine.
- Delayed period - lasts a lifetime . Prevention after surgery never ends if the patient does not want to face complications and re-infection. Every year, it is recommended to have an MRI of the cervical region, take tests, visit a physical therapist and follow general lifestyle recommendations.
Complications
Each operation can have an unfavorable outcome, which happens due to the error of the doctor or the patient himself. The risk of complications is higher with discectomy and virtually eliminated with endoscopic technique and laser vaporization.
What complications can occur after removal of a hernia of the spine:
- damage to the spinal root - leads to impaired sensitivity along the nerve and paralysis;
- infection of the wound - it happens both during the operation and in the early rehabilitation period if the rules of asepsis and antisepsis are not followed;
- allergy to the applied anesthesia, implants, suture material;
- hypersensitivity of immediate or delayed type - occurs in response to the effects of certain drugs that are intolerant, this is the most dangerous complication, without timely help it can be fatal.
Prevention
A hernia of the cervical spine can recur, but in addition to this there is a risk of many complications. To reduce the likelihood of adverse effects, after surgical treatment, you must follow a number of strict rules and adhere to general recommendations.
Prevention during the rehabilitation period has the following goals:
- elimination of pain syndrome;
- prevention of recurrence and progression of the disease;
- restoration of the function of the diseased back;
- strengthening the natural muscular corset of the spine;
- development of the ability to perform hard physical work.
To achieve maximum results, the approach to recovery should be complex with physical and mental preparation and a gradual increase in the load. Mandatory conditions for successful rehabilitation will be diet, work and rest, wearing a bandage and timely treatment of concomitant diseases.
During the rehabilitation period, there are a number of restrictions:
- it is permissible to perform any work only in a medical bandage;
- you can not sit and make sharp turns, tilts;
- osteopathic treatment is prohibited;
- you can lift no more than 3 kg;
- It is important to control weight, monitor nutrition.
Physiotherapy
After the operation, physiotherapeutic techniques are used to restore microcirculation in the operated area, relieve pain and accelerate regenerative processes. Also, physical methods will help remove the hematoma and increase muscle tone.
The doctor prescribes one or more methods of physiotherapy:
- medicinal electrophoresis;
- laser treatment;
- massage and manual therapy;
- ultrasound treatment;
- balneotherapy;
- magnetotherapy;
- mud baths;
- acupuncture;
- hirudotherapy.
A herniated cervical spine may return with minimally invasive surgery.
Strengthening the muscles that hold the spine will help reduce the risk of this. This can be done only through physiotherapy exercises, kinesitherapy, which is performed on special simulators.
Bandage
You can't do without a postoperative bandage for the first few weeks after the operation. It is needed to exclude sudden movements that can damage the diseased back. It also supports a weakened spine and performs a massage function.
The correct bandage should restrict movement, but not constrain or rub the skin. It is selected together with the doctor and worn according to the instructions of the specialist.
Exercise stress
Full recovery of the spine necessarily includes a set of exercises on simulators. They are designed specifically for dosed and safe load on each part of the back. Kinesitherapy can only be performed on special simulators, but therapeutic exercises for the spine can already be performed at home without additional devices.
In rehabilitation centers you can see simulators from DAVID and other companies. Each representative has a different appointment. For example, the F110 DMS-EVE model is considered the most significant for the patient after surgery. The simulator is used to develop the muscles of the back, chest and hips. During classes, short deep muscles are involved, which is difficult to achieve when training at home.
Gymnastics at home is no less important, and it should become a part of life, and not just the rehabilitation period. These should be regular exercises for the muscles of the back, abdomen and legs. We should not forget about the importance of spa treatment, which is recommended every year. It is useful to engage in swimming, cycling, but jumping, power sports, base jumping and similar extreme activities are excluded.