What is dangerous diaphragmatic hernia in newborns
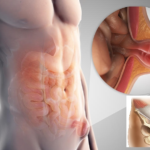
Congenital diaphragmatic hernia in children is a rare anomaly of intrauterine development of the fetus, which is characterized by the movement of the abdominal organs into the chest through the esophageal opening in the diaphragm. Such a pathology in adults is not considered dangerous, but for children this defect can cost their lives. For the first time, a diaphragmatic hernia in a fetus can be detected even during prenatal diagnosis, but washed out signs will not allow an accurate diagnosis.
Already after birth, the baby can observe specific manifestations of the pathology in the form of cyanosis, foamy discharge from the mouth, weak crying and heavy breathing.
Congenital diaphragmatic hernia begins its formation from the 4th week of pregnancy, when the wall is laid between the peritoneal and pericardial cavities. At this time, for various reasons, the development of individual muscle structures is disrupted, defects appear on the diaphragm, which become a factor in the appearance of a hernial sac with contents in the form of the stomach and part of the intestine.
Causes of congenital diaphragmatic hernia
There is no precisely established cause of congenital HH, but many risk factors are known that directly or indirectly affect the development of this pathology. A child can be diagnosed with a true and false hernia. In the first case, the hernial sac is formed by the pleural and abdominal leaf. False anomalies are manifested by the exit of organs that are not covered with a bag into the chest cavity, which provokes intrathoracic tension syndrome.
A frequent form of pathology in a child is Bogdalek's congenital diaphragmatic hernia, when the organs move through the posterior parietal defect of the diaphragm.
In addition, a diaphragmatic hernia can occur in a child after birth, then the treatment approach will be different, and the acquired form of the pathology has a favorable prognosis.
So why does a congenital diaphragmatic (CHD) hernia in a newborn:
- severe pregnancy with toxicosis;
- exacerbation of systemic pathologies in a pregnant woman;
- frequent constipation, bloating and other disorders of the digestive tract;
- respiratory diseases;
- taking medicines and narcotic drugs;
- drinking alcohol, smoking;
- severe stress, constant experiences of a pregnant woman.
Acquired diaphragmatic hernia in newborns occurs after birth in the first few months of life.
The reasons are frequent constipation, hysterical crying and a strong cry. Such a disease is associated with anomalies of intrauterine development, mainly with weakness of the thoracic diaphragm, but only this factor will not be able to start the pathological process. For the appearance of the disease, other conditions are also needed that provoke an increase in intra-abdominal pressure.
How the disease manifests itself
The abdominal organs that have penetrated through the diaphragm begin to put pressure on the lungs and heart of the baby, and therefore their formation is also disturbed. Congenital HH is often combined with other anomalies of intrauterine development, and this further exacerbates the serious condition of the newborn. More often, a left-sided hernia is diagnosed in a child, but the defect can appear anywhere.
The symptoms of the pathology will not depend on the location of the hernial orifice, but their severity is affected by the contents of the sac, its size and associated disorders. A hernia of the diaphragm will have serious consequences for the baby, regardless of the clinic, and an asymptomatic course will only aggravate the condition.
The child immediately after birth may appear completely healthy on the outside.
In this case, weak crying will be an indirect sign of pathology, because the lungs do not fully open. However, it may be difficult for the baby to breathe, and then cyanosis can already be observed. Cyanosis of the skin appears already on the first day, and the sooner this happens, the less likely it is to provide adequate assistance to the child, saving his life.
Cyanosis often occurs after several bouts of asphyxia during feeding. The child begins to choke, the skin turns blue, the muscles are tense. These manifestations subside when the baby is placed on its side from the side of the hernia. With the first attack of asphyxia, the child undergoes an X-ray examination to confirm the disease.
The main symptoms of a diaphragmatic hernia in a child:
- vomiting - does not always appear, is not a specific manifestation;
- cough - rarely occurs due to food particles getting stuck in the esophagus;
- asymmetry of the chest cavity - this indicates dextrocardia, the movement of the heart;
- superficial frequent breathing - tachypne is accompanied by tachycardia, cyanosis, bloating, violation of important reflexes.
About common symptoms of HH since birth :
- light weight and slow set;
- lack of appetite;
- pallor or blueness of the skin;
- pneumonia;
- blood in feces and vomit;
- pathology of the heart and respiratory system.
Types of HH in newborns
Congenital diaphragmatic hernia can be true and false. True, in turn, is parasternal, frenopericardial and esophageal openings. False can be traumatic, diaphragmatic-pleural. In rare cases, several forms of pathology are combined, and most often, hernias of the POD and diaphragmatic-pleural are diagnosed in babies.
To confirm the form of the disease, the child undergoes an ultrasound scan, a blood test is taken, CT, endoscopic examination, esophagogastroscopy are additionally prescribed.
Diagnosis before and after birth
Prenatal diagnosis is possible by ultrasound and magnetic resonance imaging. Both methods are safe during pregnancy and can be used repeatedly. An indirect sign of pathology is polyhydramnios due to a violation of the ingestion of amniotic fluid by the fetus.
It is rare to see a fluid-filled bowel in the chest, but the diagnosis is made when any abdominal organ is found above the diaphragm. A specific sign of the disease will be a violation of the position of the heart, which is shifted to the side. The fetus may also have dropsy due to impaired venous outflow. Differential prenatal diagnosis is carried out with such pathologies as a benign neoplasm, cyst and adenomatous transformation of the lungs.
After birth, the child is assigned x-rays. In the picture, the doctor sees areas of enlightenment in the form of honeycombs, which are located on the side of the defect. The heart is slightly displaced to the right, the dome of the diaphragm is practically not defined.
Differential diagnosis after the birth of a baby is carried out with atresia and stenosis of the esophagus, hemorrhage in the brain, neoplasms of the liver and impaired ventilation of the alveoli.
Treatment Methods
If a severe form of pathology is detected during pregnancy, treatment begins immediately. The main method of prenatal therapy is the correction of tracheal occlusion. The operation is scheduled between 26 and 28 weeks. The essence of the procedure will be the introduction of a balloon into the trachea of the fetus, which stimulates the development of the lungs. It is removed during childbirth or after the birth of the baby.
Such an operation is performed in severe pathology and only in specialized centers. The prognosis of the disease depends on many factors, and the probability of cure is 50%.
After birth, therapy begins with ventilation of the baby's lungs. The only effective method of getting rid of a hernia is surgery. Emergency intervention is performed in case of infringement and internal bleeding. The planned operation is performed in 2 stages. On the first one, an artificial ventral hernia is created to move the organs, and on the second one, it is removed with drainage of the pleural cavity.
After the operation, the likelihood of complications is high:
- General - fever, difficulty breathing, dehydration and swelling.
- On the part of the gastrointestinal tract - intestinal obstruction.
- On the part of the respiratory system - pleurisy, swelling and inflammation.
Recurrence of the disease after surgical removal often occurs after removal of paraesophageal hernias. To prevent the re-development of the pathology, the child needs to provide proper nutrition, the feeding regimen is prescribed by the doctor. In the early period of rehabilitation, the child is constantly under artificial ventilation.
Undesirable consequences of the operation occur in 15-25% of cases.
Prevention
Planning pregnancy and following certain rules during gestation is the main prevention of congenital pathologies. Before conception, it is important for a woman to rehabilitate systemic pathologies, give up bad habits and take a course of vitamin therapy.
During the period of planning and bearing the fetus are recommended :
- minimization of stressful situations , and yoga classes, meditation, breathing exercises, a visit to a psychologist contribute to this;
- balanced and nutritious nutrition , and the best option would be a diet according to a specially created program, depending on the individual needs of the body;
- moderate physical activity , regular walks, a healthy night's sleep;
- complete rejection of bad habits, namely drugs, tobacco, alcoholic and energy drinks.
An important condition for the prevention of congenital anomalies will be regular visits to the gynecologist and other doctors when the state of health changes for the timely detection of any abnormalities.